
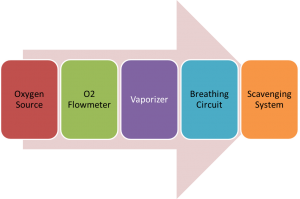
Basic components of anesthesia machine
An anesthesia machine is used to generate and mix medical gases like oxygen or air and anesthetic agents for the purpose of inducing and maintaining anesthesia in patients. The basic components of anesthesia machine and delivery system consists of
- Source of oxygen (O2) – The source of oxygen may be a central distribution system / pipeline or pressurized tanks / cylinders,
- O2 flowmeter – This device uses an adjustable needle valve to deliver the desired flow of oxygen in ml or liters per minute to the patient breathing circuit,
- Vapourizer – A device which produces a vapor from a volatile liquid anesthetic. Halogenated anesthetics include isoflurane, halothane, enflurane, desflurane, sevoflurane and methoxyflurane.
- Patient Breathing Circuit (tubing, connectors and valves) – The patient breathing circuit is the channel for anesthetic gas delivery to the patient. The function of breathing circuit is to deliver a mix of oxygen and anesthetic gases and eliminate carbon dioxide from the exhaled air. Carbon dioxide may be eliminated by either additional fresh gas flow (FGF) or by soda lime absorption. The breathing circuit also provides for assisting or controlling ventilation, if needed.
- Scavenging System – device that removes any excess anesthetic gases. Removing excess anesthetic gases is critical since room pollution with anesthetic gases may lead to health problems in other people in the environment.
Anesthesia delivery process
The process of anesthesia starts with the oxygen flow from pipeline or cylinder through the flowmeter. O2 flows through the vapourizer and picks up the anesthetic vapors. The O2-anesthetic mix then flows through the breathing circuit and into the patient’s lungs, usually by spontaneous ventilation or normal respiration. When the oxygen is turned on, the gas flow is continuous, as follows:
The Boyle′s machine has been the most frequently used anesthesia machine since it was developed in early 20th century. This is a continuous-flow anesthesia machine, which is designed to provide a specific supply of medical gases mixed with a specific concentration of anesthetic vapour and deliver this continuously to the patient at a specific pressure and flow. When necessary, mechanical ventilation could be used depending on the patient condition.
However with basic anesthesia machines, the following types of issues were faced:
- Higher degree of wastage of gases and anesthetic agents.
- Machines were completely mechanical systems with semi-open circuits and high fresh gas flow.
- There were multiple connections, prone to disconnection, misconnection, kinking, leakage or obstruction.
- Accuracy of flow meters was poor.
- There were no performance feedback mechanisms such as alarms.
- Mechanical ventilation burdened the anesthetist especially in case of more critical patients.
- Accuracy of anesthesia delivery and efficiency of the system was low and as a result patient safety often compromised.
Early on it was recognized (at the cost of many unfortunate patient lives), that accurately controlling the amount of anesthetic agent and oxygen delivered and maintaining ventilation of the lungs with oxygen enriched gas was critical to the safety of the patient and also that this was not always achieved efficiently and accurately through continuous flow or completely mechanical anesthesia units. Therefore, there have been consistent attempts by manufacturers to improve the design of these machines in order to achieve the above objectives.
Developments in anesthesia machine
Subsequently anesthesia machine were developed with a view to significantly improve patient safety and efficiency of the machine. They included additional components of anesthesia machine and features with the intention to:
- Improve accuracy of gas and anesthetic mix delivered to patient – e.g. Flowmeters with Hypoxic guard and fail-safe. If the oxygen is depleted/low, the fail-safe mechanism also reduces the nitrous oxide flow to prevent a hypoxic gas mixture from being delivered to the patient (Oxygen should be 21% or more as per anesthetist requirement, never less). It will also assure that when the flow of nitrous oxide is increased, the flow of oxygen will be increased concurrently. Other safety features include Pin indexing, colour-coding, Non-Interchangeable Screw Thread or Diameter Index Safety System, Non-interchangeable Scrader valve etc., so that no mix-up of gases occurs even inadvertently. E.g. Datex Ohmeda Excel 210 SE anesthesia machine supports Pin-Indexed, Gas-Specific Dual O2 and N2O Flowmeters.
- Reduce leakage – Pressure gauges, regulators and ‘pop-off’ valves, to monitor gas pressure throughout the system and protect the machine components and patient from excessive rises.
- Assisted ventilation instead of manual ventilation – easing out the anesthetists and giving them capability to handle more critically ill patients. Bellows ventilator type: Mostly, all anesthesia workstations include either a hanging bellows or standing bellows. A standing bellows collapses immediately if there is a leak in the machine or if the patient becomes disconnected. A hanging bellows continues to refill even if there is a substantial leak. Most modern machines have a standing bellows ventilator as it gives visual alarm about disconnect leakage or lower gas levels. If one chooses the hanging bellows option, as an extra precaution, you may want to purchase a machine with a disconnect alarm to warn the anesthesiologist, as visual indication will not be there.
- Patient monitoring for multiple parameters – Systems for monitoring the patient’s heart rate, ECG, blood pressure and oxygen saturation, end-tidal carbon dioxide and temperature are included. Patient monitoring is critical among the various components of anesthesia machine.
- Breathing Circuits with Circle System – Most anesthesia machines feature circle system for better efficiency. This ensures reuse of excess oxygen and anesthetic agents rather than complete waste as in an open circuit.
Still some of the older anesthesia machines had problems like:
- Most anesthesia ventilators were ′bag in bottle′ machines that consume oxygen for powering the ventilator to deliver tidal volume and wasted lot more oxygen.
- Internal positive end-expiratory pressure (PEEP) valve is absent and one might need to use an external PEEP valve having its own risks.
- Advanced modes of mechanical ventilation were not available with old generation ventilators, which made handling more critically ill patients riskier for anesthetists. E.g Datex Ohmeda Aestiva 5 anesthesia machine supports volume control mode, but pressure control mode is optional.
- Integrated volume and pressure monitors were not there, exposing patients to the risk of unnoticed leaks or disconnections causing trauma to patient. They are unable to deliver tidal volumes with accuracy.
- Leakage and safety checks were to be done largely manually.
- Systems were largely mechanical or pneumatic. This had the disadvantage of higher degree of user intervention as compared to latest electronic system, but users did feel more in control and had the advantage of not overly relying on electricity or battery back-up availability.
On the whole each one of components of anesthesia machine, i.e gas delivery, ventilation and patient monitoring etc. worked independently with limited integration. It was largely left to the anesthetist to process & assimilate all information from each component while handling the patient and charting and maintaining records.

Advent of Integrated Anesthesia Workstation
Over time, the conventional anesthesia machine has evolved into an Advanced Carestation or anesthesia workstation. The workstations offer integrated advanced patient monitoring, use advanced electronics, software and technology ensuring advanced capabilities for ventilation, monitoring, inhaled agent delivery, low-flow anesthesia and closed-loop anesthesia. They could be seamlessly integrated with Electronic Medical Records and Hospital Information Systems.
Due to high degree of integration between gas delivery system, ventilator and monitors – it is possible to deliver tidal volumes accurately and eliminate several hazards associated with the low pressure system and oxygen flush. Appropriate use can result in enhanced safety and economy of anesthetic delivery and monitoring.
However, these workstations pose their own new challenges. The main issues being that since the workstations are advanced electronic systems, the staff needs to be thoroughly trained in their usage. Staff used to older systems that consist of basic components of anesthesia machine, may find the advanced systems complex and intimidating. Systems differ from each other in their design and operation, hence having a mix of different workstations in the same facility often confuses staff and results in more human errors.
The Modern Anesthesia Workstation
The modern anesthesia workstation is an integrated unit consisting of the following components:
- Basic components of anesthesia machine unit (including gas delivery, electronic flowmeters, vapourizers, breathing circuit, scavenging system)
- Advanced Ventilation
- Anesthesia and patient monitoring system
- Integration with Electronic medical records
Some of the feature advancements in the latest workstations as compared to earlier generation anesthesia machines are as follows:
Electronic Flow Meters
Sophisticated pressure transducers and electronically controlled flow control valves ensure better accuracy of gas delivery. Electronic flowmeter are not only more accurate but also do not have problems related to multiple mechanical parts which are prone to leaks and breakages. The information related to the flow may be displayed either in digital or virtual form. Some machines like Drager Fabius GS have conventional control knobs and flow control valves but flow data is displayed electronically using electronic flow sensors and digital displays rather than glass flow tubes. These allow easier visualization and control of flow and also allow export of electronic data to an information system. In some fully electronic systems, the flow control is also electronic. In some machines mechanical flow meters are also provided to deliver oxygen in absence of electrical power. Integrated software control gas flow and vapourizer output so as to achieve best economy of gases.
Breathing Circuit – Circle system
Modern anesthesia machines feature circle absorber system rather than open or semi-open circuits, essentially designed for low flow anesthesia. Misconnections or disconnections are reduced and compact circuits enable rapid changes in gas composition at low flows. Water-vapour or moisture conservation is better. Vertically mounted unidirectional valves introduced in some newer models decrease resistance to flow. Disposable units of Carbon dioxide (CO2) absorbers and bypass valve are available so as to ensure replacement without disruption of anesthesia gas delivery, leakage or change in gas mix.
Ventilator – Advanced ventilation modes & electronic piston driven
Ventilators are one of the most important components of anesthesia machine. Newer systems come with ventilators that use electrically driven pistons or turbines to generate flow instead of pressurized oxygen in traditional ventilators. This saves oxygen considerably and can be used only for the patient breathing circuits.
Modern anesthesia machines are equipped with technology and features present in advanced intensive care unit ventilators. Ventilation modes such as pressure support ventilation (PSV) and volume assist ventilation have been introduced to support ventilation in patients maintained on spontaneous breathing through a Laryngeal Mask Airway. In addition, synchronized intermittent mandatory ventilation (SIMV) breaths can be added to both pressure and volume controlled ventilation. E.g. Drager Fabius GS Anesthesia workstation supports all modes like pressure, volume control, SIMV etc. Some provide apnea backup in the pressure support mode as a safety feature. Thus, modern anesthesia ventilators can be used for even complicated patient cases also.
A major advancement has been intraoperative ventilation between gas delivery system and ventilator that has enhanced the ability to deliver very low tidal volumes accurately. This cannot be achieved through a modular approach. This high degree of accuracy has also been achieved due to additional features in modern machines such as:
- More precise piston ventilators than bellows ventilators.
- Fresh gas decoupling (FGD) or electronic compensation for fresh gas augmentation of tidal volume.
- Performance of self-test capability, which quantifies leak and compliance of the patient and ventilator circuit. Compliance compensation enables delivery of tidal volumes as low as 20 ml with accuracy.
Still some systems parallelly have mechanical ventilation with smooth switch option. E.g GE S/5 Aespire 7900 has one step mechanical bag to vent switch that turns ventilator on/off and requires no electronics to do that.
Target Controlled Anesthesia
The fully integrated and automatic system has provided Target Controlled Anesthesia (TCA) capabilities. With TCA capability the anesthetist can set the target end-tidal oxygen and anesthetic agent values and the integrated system constantly monitors these values and automatically adjusts the gas delivery and total flow in order to maintain the set target values. Smart in-built safeguards help protect against over-delivery and under-delivery of agent and hypoxia. This provides cost-effective anesthesia by keeping gas and agent consumption to an absolute minimum.
Total intravenous anesthesia
The alternate method to inhalational anesthesia is providing total Intravenous Anesthesia. This could also highly automated with a software system integrating data from anesthesia system, drug database and feeding into syringe pumps to automatically set dosages for drugs being administered, e.g. Drager Zeus.
Monitoring systems
Integrated anesthesia and patient monitoring systems has been one of the most significant advancements in anesthesia workstations. The monitoring systems have been marked with sophisticated visual and audio electronic alarms, categorised based on the urgency of situations and several new monitoring capability e.g., complex respiratory waveforms.
Most modern anesthesia monitoring systems have flexible display screen that can be configured according to preferences from extensive clinical parameters that include hemodynamic, respiration and ventilation monitoring, temperature, anesthesia depth monitoring and anesthesia gas monitoring. Certain monitors also provide monitoring of muscle relaxation. These monitors have plug in parameter modules that can be inserted and removed without interrupting other monitoring. Built-in connectors and communication software permit optional cardiovascular and respiratory gas monitoring. E.g. in Drager Narkomed 6400 anesthesia workstation. Many of these monitors are capable of giving graphical as well as numerical trend of vital parameters for the past 24 hours.
ECG monitors are equipped to display multi-lead ECG with ST-segment analysis and arrhythmia recognition for advanced monitoring of a cardiac patient. SpO2 and EtCO2 are standard. In hemodynamic monitoring along with automated non-invasive blood pressure monitoring, one can monitor invasive pressure like central venous pressure, arterial pressure or pulmonary arterial pressure. Most of these monitors are also equipped with cardiac output monitoring.
As more and more anesthesia workstations have capability of advanced ventilation, one can also monitor ventilator parameter including compliance, auto PEEP and various loops (flow volume/pressure volume) and graphs (pressure-time, flow-time or volume-time). Other parameters that can be monitored include anesthesia depth, end-tidal concentration of various anaesthetic agents, inspired and expired oxygen concentration and temperature.
Respiratory monitoring includes spirometry – displayed using flow sensors in the expiratory limb near the unidirectional valve or at the Y piece in certain models and flow time and flow volume waveforms which are essential for ventilating diseased lung in addition to the pressure time and volume time waveform.
Automatic machine testing
In older anesthesia machines leaks, misconnections or disconnects would have to be manually checked. This may not be regularly or properly done. Most modern anesthesia delivery systems perform some degree of self-test and have ability to detect and report many faults if not all, such as valve failure.
Automated record keeping
Anesthesia Information Management System consist of a combination of hardware and software that interface with intraoperative monitors and automatically record data from the monitors like vital signs and ventilator parameters for charting purposes. This could be integrated and be part of the hospital information system and Electronic medical records.
E.g. The Datex Ohmeda S5 ADU Carestation utilizes electronic control for both gas delivery and vaporization. The automatic data capture from these systems as well as ventilator not only avoids manual documentation but also allows anesthesia and patient vitals monitoring & display extensively. The ADU Carestation can be linked, through the Datex-Ohmeda Anesthesia Monitor, to a network of other carestations and with the hospital information systems/ electronic medical records of the patient.
Power back-up
Since all modern workstations have more complex electronically controlled systems they depend heavily on continuous supply of electricity and have battery backup. It is important to know the extent and duration of battery back-up available, so that in case of power failure suitable manual back-up mechanisms are kept ready.
Some of the safety and operational features present in newer machines may be absent in older machines. However, they were designed to be operated without much electricity, using compressed gas power for the ventilator and suction apparatus. Modern machines which are highly electronic, need battery backup in every component, which can be only for a limited period of time, say 30 minutes. When faced with budgetary constraints and potentially limited utilization, one may not be in a position to go for an advanced full-fledged anesthesia workstation. In which case, a thorough approach to features comparison would be necessary to make the right purchase.
Read more about what to look for when buying an anesthesia system for your hospital – How to choose the right anesthesia machine for your hospital?
Primedeq offer various refurbished and used anesthesia machine options with warranties. Click here for more details.
https://in.linkedin.com/in/shanthi-mathur-ab07838
