Image Credit: researchgate.net
“My neighbour has been detected Covid-positive and admitted to nearby hospital”, reported a WhatsApp group member a few days back. Another member enquired if she was on ventilator? The first member replied she was actually on ‘Oxygen Therapy’. A third member chimed in, saying, “Oh! that is not too bad. My Mother has been using Oxygen concentrator for nearly 2 years now.” Another knowledgeable member commented, “It’s not the same. Oxygen concentrator is Low Flow Oxygen Therapy and what hospitals are using to treat acute patients, is High Flow Oxygen therapy.”
Everyone else wondered, what exactly was the difference between Ventilator and Oxygen therapy – High Flow or Low Flow?!
Everyone knows being on ventilator is serious. How serious is being on oxygen therapy?
Oxygen Therapy vs Ventilation in COVID19
Oxygen therapy has become the buzz-word in treatment of COVID19 patients in recent months. March-May 2020 saw a mad scramble for Ventilators in India and all over the globe. Governments and people around the world learnt about how COVID19 could lead to lowering of oxygen saturation in the body very silently. It was noticed that some breathless patients had oxygen saturation or SpO2 levels reduced to even 50-60%, by the time they reached Hospital Emergency Room without feeling much else.
The normal oxygen saturation range is 94-100%. Oxygen saturation <94% is described as ‘Hypoxia’. Hypoxia or Hypoxemia could result in breathlessness and lead to Acute Respiratory Distress. Everyone largely assumed Ventilators were the answer for acute Covid19 patients. However, lately statistics have shown that only approximately 14% of individuals with COVID-19 develop moderate to severe disease and require hospitalization and oxygen support, with only a further 5% who actually require admission to an Intensive Care Unit and supportive therapies including intubation and ventilation.
In other words 86% of those who tested positive for COVID19 are either asymptomatic or show mild-to-moderate symptoms.
These people neither need oxygen therapy nor ventilation, but the 14% mentioned above do. WHO recommends supplemental oxygen therapy immediately for patients with respiratory distress, hypoxia/hypoxaemia or shock. The aim of oxygen therapy is to get their oxygen saturation level back to >94%.
What you need to know about High Flow Oxygen Therapy
Just in case you or your loved one happens to be in the 14% category mentioned above – you may want to know more about oxygen therapy.
- You may want to know how oxygen therapy is different from ventilator.
- What are the various oxygen devices and delivery systems?
- How do they work? What are the various components?
- How are these devices different in their capabilities?
- How do they differ in their benefits and risks?
- What are the indications – Who needs oxygen therapy and who requires Ventilator?
Read on to know more…
How is an oxygen therapy device different from a ventilator?
To understand how an oxygen therapy device is different from a ventilator, we must first understand the difference between Ventilation and Oxygenation.
Ventilation vs oxygenation
Ventilation – Ventilation is the activity of normal, spontaneous breathing, including the processes of inhalation and exhalation. If a patient is unable to do these processes on their own, they may be put on a ventilator, which does it for them.
Oxygenation – Ventilation is essential for the gas exchange process i.e oxygen delivery to the lungs and carbon dioxide removal from the lungs. Oxygenation is only the first part of gas exchange process i.e. delivery of oxygen to the tissues.
Difference between High Flow Oxygen therapy and Ventilator in essence is the following. Oxygen therapy involves only giving you additional oxygen – your lung still does the activity of taking oxygen-rich air in and breathing carbon-di-oxide rich air out. A ventilator not only gives you additional oxygen, it also does the work of your lungs – breathe in & out.
Who (What type of patient) needs Oxygen therapy & who needs ventilation?
In order to apply the appropriate treatment, one needs to determine whether the issue with the patient is poor oxygenation or poor ventilation.
Respiratory Failure could occur due to
- an oxygenation issue resulting in low oxygen but normal – low levels of carbon dioxide. Also known as hypoxaemic respiratory failure – this occurs when the lungs are unable to absorb oxygen adequately, generally due to acute lung diseases that cause fluid or sputum to occupy the alveoli (Smallest sac-like structures of the lung which exchange gases). Carbon dioxide levels may be normal or low as the patient is able to breath-out properly. A patient with such a condition – Hypoxaemia, is generally treated with oxygen therapy.
- a ventilation issue causing low oxygen as well as high levels of carbon dioxide. Also known as hypercapnic respiratory failure – this condition is caused by patient’s inability to ventilate or breathe-out, resulting in carbon-di-oxide accumulation. CO2 accumulation then prevents them from breathing-in adequate oxygen. This condition generally requires support of ventilator to treat patients.
Why are Low Flow Oxygen Therapy devices not adequate for acute cases?
In acute cases why do we need high flow oxygen therapy rather than use simple oxygen concentrators?
The tissues in our body require oxygen for survival. Shortage of oxygen or hypoxia in the tissues for a long time (more than 4 minutes) could cause serious injury eventually leading to fatality. While a physician could take some time to evaluate the underlying causes, increasing oxygen delivery meanwhile could prevent death or disability.
A normal adult breathes in 20-30 litres of air per minute under moderate activity level. 21% of air we breathe-in is oxygen, i.e about 4-6 litres/minute. The FiO2 or fraction of inspired oxygen in this case is 21%.
However, in acute cases the solubility of oxygen in blood could be low. Even when the inspired/inhaled oxygen concentration is 100%, dissolved oxygen may provide only one third of resting tissue oxygen requirements. Therefore, one way to address tissue hypoxia is to increase the fraction of inspired oxygen (Fio2) from the normal 21%. In many acute conditions, inspired oxygen concentrations of 60-100% for short periods (even upto 48 hours) may save life until more specific treatment can be decided and given.
Suitability of Low Flow Oxygen Devices for Acute Care
Low flow systems have flow lower than inspiratory flow rate (Normal inspiratory flow is between 20-30litres/minute as mentioned above). Low flow systems such as oxygen concentrators generate flow rates of 5-10 litres/m. Even though they offer oxygen concentration up to even 90%, since the patient needs to inhale room air to make-up for the balance inspiratory flow requirement – the overall FiO2 may be better than 21% but still be inadequate. Additionally, at low oxygen flow rates (<5 l/min) significant rebreathing of stale exhaled air may occur because exhaled air is not adequately flushed from the face mask. This results in higher retention of carbon dioxide and also reduces further intake of fresh air/oxygen.
Also when oxygen is delivered at a flow rate of 1-4 l/min by mask or nasal prongs, the oropharynx or nasopharynx (airways) provides adequate humidification. At higher flow rates or when oxygen is delivered directly to the trachea, additional external humidification is required. Low flow systems are not equipped to do so. Additionally, FiO2 cannot be accurately set in LF.
On the whole low flow oxygen systems may not be suited for acute cases of hypoxia.
Suitability of High Flow Oxygen Devices for Acute Care
High Flow systems are those that can match or exceed the inspiratory flow rate – i.e 20-30 litres/minute. High Flow systems available today can generate flow rates anywhere between 2-120 litres/minute much like ventilators. FiO2 can be accurately set and monitored. FiO2 can be nearly 90-100%, since the patient need not breathe any atmospheric air and loss of gas is negligible. Rebreathing of expired gas is not a problem because the mask is flushed by the high flow rates. They also enhance patient comfort by maintaining moisture and adequate heat in the gas to lubricate the nasal passage.
Overall, high flow systems can not only improve oxygenation as required in acute cases, but also reduce the work of breathing, causing much less strain to patient lungs. Hence they are well suited for this purpose in acute cases of respiratory distress.
What are the Components of a High Flow Nasal Cannula vs Ventilator?
We have seen that at least a high flow oxygen therapy (HFOT) system is required to treat acute respiratory failure cases. Let’s examine how a High Flow (HF) system differs from a ventilator. What are the various components of the both the machines and how do they differ in their functioning?
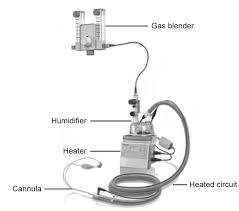
Both machines need to be connected to an oxygen source in the hospital like the pipeline or cylinder. A high-flow oxygen therapy system is simple – consisting of a
- flow generator,
- an air-oxygen blender,
- a humidifier,
- heated tube and
- a delivery device e.g. a nasal cannula.
Ventilator workings
A ventilator on the other hand is more extensive. It not only consists of all the components of a HFNC, it additionally has breathing, control and monitoring systems along with and alarms to perform safe, controlled, programmable ventilation for the patient.
The most important parameters to program in mechanical ventilation are:
- The ventilation mode, (volume, pressure or dual),
- Modality (controlled, assisted, support ventilation), and
- Respiratory parameters. The main parameters are tidal volume and minute volume in volume modalities, peak pressure (in pressure modalities), respiratory frequency, positive end expiratory pressure, inspiratory time, inspiratory flow, inspiratory-to-expiratory ratio, time of pause, trigger sensitivity, support pressure, and expiratory trigger sensitivity etc.
Alarms – To detect problems in the ventilator and changes in the patient, alarms for tidal and minute volume, peak pressure, respiratory frequency, FiO2, and apnea are available.
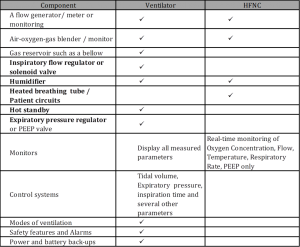
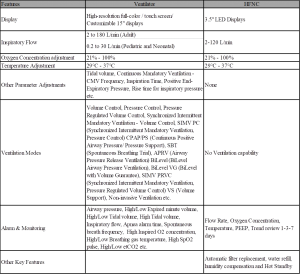
The basic component comparison of a ventilator and HFNC
Feature comparison between Ventilator and HFNC
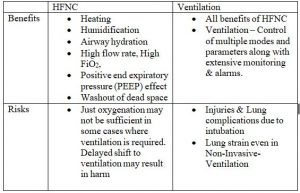
Ventilation vs HFNC – Benefits and Risks
Ventilation could be Invasive or Non-invasive. In case of invasive ventilation a tube is inserted through mouth to the lungs to assist in ventilation. Physicians like to avoid intubation as far as possible due to the potential deleterious effect on the patient and difficulty in managing them.
Intubation while not serious in itself, may cause
- Injury to lungs, trachea or throat etc. and/or
- There could be risk of
- Fluids build-up,
- Aspiration or
- Lung complications.
Non-invasive ventilation
Non-invasive ventilation is a preferred option as far as possible. NIV provides assistance of the spontaneous ventilation by applying positive pressure into the lungs externally, through a commonly used face mask connected to a humidification system, a heated humidifier or a heat and moisture exchanger, and a ventilator. The most commonly used mode combines pressure support (PS) ventilation plus positive end-expiratory pressure (PEEP), or simply apply continuous positive airway pressure (CPAP). The pressure support is variable depending on whether the patient is breathing in or out and their breath effort.
NIV improves gas exchange and reduces inspiratory effort through positive pressure. It is called “non-invasive” because it is delivered without any intubation. NIV may however result in high tidal volumes promoted by pressure support and that may potentially worsen pre‐existing lung injury.
Advantage of HFNC
The other advantage of delivering high flow oxygen through a nasal cannula is to continuously flush out the upper airway dead space by better CO2 clearance. This reduces work of breathing for the patient and improves oxygenation. In addition, high flow oxygen therapy ensures high FiO2. HFNC provides good patient comfort through heated and humidified gas flow delivered via nasal prongs at a steady rate. The constant flow rate of gas in the HFNC system generates variable pressures in airways according to the patient’s breath effort. Compared with conventional (Low Flow) oxygen therapy or noninvasive ventilation, the use of high flow oxygen therapy may reduce the need for intubation.
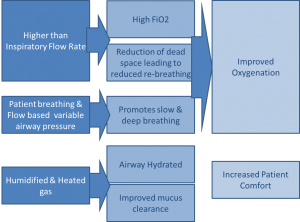
Treatment strategies for patient with acute respiratory condition are aimed at providing adequate oxygenation. At the same time it is important to preserve or strengthen patient’s lung activity without straining respiratory muscles.
HFOT might therefore be considered as a first‐line strategy of oxygenation in these patients. However, to avoid any harm due to delayed ventilation/ intubation, constant monitoring is crucial.
Summary of benefits and risks of HFNC vs Ventilation
Use of HFNC and ventilators in treatment of COVID
Roughly 15% of the COVID19 cases are estimated to need oxygen therapy and a little less than 1/3rd of them may have to move to ventilation. As mentioned earlier critical care givers avoid intubation as far as possible. Oxygen therapy is considered the first line of respiratory support for cases of hypoxia. HFNC demand has therefore gone up in recent months. Popular brands of HFNC in the market are Fisher & Paykel, Hamilton, Resmed, BMC etc.
PrimedeQ is an eMarketplace for medical equipment. We also assist in medical equipment repair & maintenance services at www.Primedeq.com. Contact us at +918971223957 or +917019759765 for all your medical equipment related needs.
https://in.linkedin.com/in/shanthi-mathur-ab07838