
Most Eye hospitals are set-up with a view to check general visual acuity and screen for all types of problems and diagnose & treat refractive errors, cataract and glaucoma. The reason is, these are eye problems most commonly found. Based on these cases, the most common medical equipment for eye hospital are Ophthal chair unit, autorefrator/ retinoscope, ophthalmoscope, tonometer, slit lamp, operating microscope, phaco machine, A-Scan machine along with the basic OPD and OT set-up as described further in this blog.
Download a list of equipment required for Eye Hospital with cost estimates @ just Rs 500.
Download Eye Hospital Equipment List for just Rs 500
Investment in all other equipment detailed here are dependent on the case-mix of other advanced cases received by the hospital or skills of the ophthalmologists present.
Introduction
Ophthalmology deals with diseases of the eye or parts of the eye. Some of the most common diseases that eyes are examined for and treated by Ophthalmologists include:
- Refractive error
- Cataract
- Glaucoma
- Macular degeneration
- Diabetic retinopathy
- Dry eyes
- Strabismus (squint)
- Proptosis (bulged eyes)
- Excessive tearing (tear duct obstruction)
- Uveitis or inflammation of the the pigmented layer between the retina and the outer fibrous layer composed of Sclera and Cornea.
- Eye tumors etc.
A typical large Eye Hospital is equipped to screen, diagnose and treat the above most common diseases of the eyes. However, smaller hospitals and those on a budget focus on the most common diseases and limit their investments into equipment accordingly to cater to high volume cases.
- The top three conditions leading to visual impairment are known to be refractive errors, cataract and glaucoma.
- The top three diseases leading to blindness are said to be cataract, glaucoma and macular degeneration.
Therefore most hospitals are set-up with a view to check general visual acuity and screen for all types of problems and diagnose & treat refractive errors, cataract and glaucoma.
Based on these cases, Ophthal chair unit, autorefrator/ retinoscope, ophthalmoscope, tonometer, slit lamp, operating microscope, phaco machine, A-Scan machine along with the basic OPD and OT set-up as described further in this blog, are the common medical equipment for eye hospitals invest in. Investment in all other equipment detailed here are dependent on the case-mix of other advanced cases received by the hospital or skills of the ophthalmologists present.
What are the eye examinations and related medical equipment required to screen, diagnose and treat the most common diseases of the eye?
Eye examination/ Diagnostic Medical Equipment for eye hospital
A thorough basic eye examination may include some of the following tests:
- Visual acuity
- Refraction
- Pupil function
- Ocular motility
- External examination
- Slit-lamp
- Visual field testing
- Intraocular pressure
- Retinal examination
- Fundus photography
Visual acuity
Visual acuity (VA) is a measure of the ability of the eye to distinguish shapes and the finer details of objects at a given distance. The standard definition of normal visual acuity (20/20 or 6/6 vision) is derived from standardized sized objects that can be seen by a “person of normal vision” at the specified distance. One has 20/20 visions, if one can see at a distance of 20 ft an object that can normally be seen at 20 ft by most with normal vision. If one has trouble seeing objects at a distance, say you can see only upto 20 ft what a person with normal vision can see out to 30 ft, then you have 20/30 vision. Visual acuity is examined using an eye chart.
Refraction
Refractive error is an optical abnormality due to which sharp focus of the image being seen, fails to be captured on the retina, falling either before or behind, resulting in blurred or distorted vision. Common vision problems such as myopia (nearsightedness) or hyperopia (farsightedness) and astigmatism are the result of refractive error. Refraction is the procedure by which the doctor finds out ideal correction of refractive error. A refraction procedure could be objective or subjective.
Objective Refraction
Objective refraction is obtained using a retinoscope or auto-refractor, without receiving any feedback from the patient.
In case of retinoscopy, the doctor projects a streak of light into the patient’s pupil. A series of lenses are changed in front of the eye. By looking through the retinoscope, the doctor can study the light reflex of the pupil. Based on the movement and orientation of this retinal reflection, the refractive state of the eye is measured.

An auto-refractor is a computerized instrument that shines light into an eye. The light travels through the eye, to the back of the eye and back to front again. The information received back by the instrument gives an objective measurement of refractive error without asking the patients any questions.
Autorefractors are one of the must-have medical equipment in eye hospital. They are not only used to measure the degree of refractive error in the eye but are also well-suited for differentiating corneal from lenticular aberrations, as well as assessing pre-and-post refractive surgery patients. The patient focuses their vision on a target such as an image of floating hot-air balloon. Like many ophthalmology instruments, they have spherical and cylindrical measurement ranges of -30 to +25D/±10D respectively. Autorefraction and keratometry may be done together. A keratometer or an ophthalmometer measures the curvature of the anterior surface of the cornea and helps in the assessment of the extent and axis of astigmatism.
When performed by an experienced clinician, retinoscopy has been found to be more accurate than automatic refraction, giving a better starting point for further investigations.
Subjective refraction
A subjective refraction requires responses from the patient. Typically, the patient will sit behind a refractor/phoropter or wear a trial frame and look at an eye chart. The optometrist changes lenses and other settings while asking the patient for feedback on which set of lenses give the best vision.
Pupil function/ Ocular motility/ External examination
A general physical eye examination includes checking the pupil function, ocular motility (alignment of the eyes, to check ‘squint’) and external examination of eyes consisting of inspection of the eyelids, surrounding tissues and palpebral fissure.
Slit Lamp examination
Slit lamp is one of the most commonly requested medical equipment for eye hospital. The slit lamp exam helps do a comprehensive eye exam. The patient sits in a chair facing the slit lamp with their chin and forehead resting on a support. The slit lamp exam, also known as biomicroscopy, combines a microscope with a very bright light. The doctor can use this instrument to observe the eyes in detail and determine existence of any of large number of abnormalities.
What does a slit lamp exam show? A slit lamp exam shows the ophthalmologist the various structures within the eyes, including the Conjunctiva, Cornea, Eyelids, Iris, Pupil, Lens, Sclera and the Retina. After an initial simple examination of the eyes, the doctor may apply a special dye called fluorescein to the eyes and a series of eye drops that will dilate the pupils to repeat and examine the back of the eyes further. A range of conditions can be detected by carrying out a slit lamp exam, such as:
- cataracts,
- corneal injury/ disease
- damage to the sclera
- a detachment of the retina
- damage to the retina or the blood vessels connected to it
- macular degeneration
- disease or swelling of the middle layer of the eye
- glaucoma
- bleeding or presence of foreign body in the eye
Examination of the Retina
Optical coherence tomography (OCT) uses light waves to take cross-section images of the retina. OCT is a safe, non-invasive diagnostic imaging test. While retinal examination can be done through slit lamp or fundus camera, with OCT, the ophthalmologist can see each of the retina’s distinctive layers. This allows him/her to map and measure their thickness. These measurements help with diagnosis and also provide treatment guidance for glaucoma and diseases of the retina. These retinal diseases include age-related macular degeneration and diabetic retinopathy.

Fundus photography
Fundus photography involves photographing the fundus or back of the eye, using fundus cameras. The main structures that can be visualized on a funduscopy are the central and peripheral retina, optic disc and macula. This procedure can be performed with colored filters, or with specialized dyes for better clarity and images.
Intraocular pressure (IOP)
Intraocular pressure is the fluid pressure inside the eye. Applanation Tonometry is the method used to determine Intraocular Pressure. Intraocular pressure is important determinant of glaucoma. Most tonometers essentially measure pressure in millimeters of mercury (mmHg). In applanation tonometry, the cornea is flattened and the IOP is determined by varying the applanating force or the area flattened. Hand held tonometer may be used in case a person has difficulty sitting and being examined on a slit lamp, for various reasons.
Visual Field Testing
Humphrey Field Analyzer – is an instrument used to test the complete visual field. It is said to be the gold-standard to measure the peripheral vision and is extremely popular in detecting glaucoma.
Ophthalmoscopy
An Ophthalmoscope is used to look at the inside of the eye. Through ophthalmoscopy several eye diseases such as glaucoma, high blood pressure damage, retinal detachment, diabetes, eye tumors etc., can be screened. The handheld instrument that a physician uses to look into the eyes is called a direct ophthalmoscope. A direct ophthalmoscope provides good, but limited visualization of the back of the eye. However, the viewer must be very close to the face of the patient, looking straight into the eye. An indirect ophthalmoscope is mounted on the head of the viewer and a condensing lens is held close to the eye. It provides the viewer a much wider field of vision of the back of the eye including elevation and depth like a 3D picture. The viewer can be arms-length away, instead of looking into the eye, giving them better control of the view. Because of this advantage, almost all eye examinations by ophthalmologists today utilize the indirect ophthalmoscope.
Pre-surgical, Surgical and Post-surgical equipment
A-Scan / B-Scan
Biometry or A-scan and B-scan are ultrasonography devices used widely in ophthalmology. A-scan ultrasound is most commonly used for measurement of axial length (AL), which is critical for intraocular lens (IOL) calculations before cataract surgery. Accurate measurement of the eye’s Axial Length is essential for attaining excellent refractive outcomes after cataract surgery, otherwise the patient would have to wear corrective eyeglasses even after surgery.
Another application of A-scan is to determine the ultrasonic properties (i.e., high internal reflectivity, low internal reflectivity) and size of posterior segment masses, which is used in conjunction with B-scan imaging to detect different types of lesions.
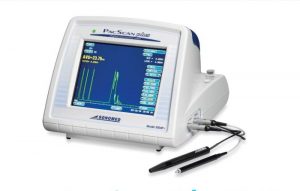
B-scan ultrasound is a two dimensional, cross-section brightness scan. It is typically used to evaluate posterior segment and orbital pathology, particularly when the ocular media are cloudy and a direct view is not possible. High resolution B-scan uses higher frequency probes (20-50 MHz vs. the standard 10 MHz) to provide detailed images of anterior segment structures, especially the angle, iris, and ciliary body.
A-scan is still especially useful in patients with mature or dense posterior subcapsular cataracts and central corneal scars. Optical Biometry equipment like IOLMaster 500 Biometer from Carl Zeiss Meditec and LENSTAR LS 900 Optical Biometer from Haag-Streit are also used for measurement of AL.
Ophthalmic microscope
The human eye is extremely delicate, hence performing ophthalmic surgery requires the ability to monitor progress on a micro-level. Ophthalmic operating microscopes are designed to provide high contrast and detailed imaging of all regions of the human eye. Special attention needs to be given to the lens. An apochromatic lens provides high light transmission, resulting in high-quality imaging even at lower light intensities. Some models of ophthalmic surgical microscopes provide multiple lighting options such as the ability to switch between halogen and xenon, they could be fixed or adjustable, and some models provide a second “observer” set of binoculars, some of which can independently adjust the focusing mechanism.
Phaco machine
Phacoemulsification is most popularly used cataract surgery procedure in which the eye’s internal lens which has developed cataract, is emulsified with an ultrasonic hand-piece and aspirated from the eye using a Phaco machine. Phacoemulsification cataract surgery is followed by the insertion of an intraocular lens (IOL). Cataracts are the most common surgical procedure done in the eyes. Hence Phaco machine is the most common medical equipment for eye hospital in the OT along with the operating microscope.
Ophthalmic Yag Laser

During a cataract operation, a new plastic lens is put inside the lens membrane (called the bag or capsule) in eye, after removing the clouded original lens. In some patients, the capsule may thicken after surgery and becomes cloudy within a couple of year or even a few months. This again obstructs the light from reaching the retina. In a Yag laser capsulotomy a laser beam is applied to the capsule creating a small hole in the centre of the capsule, to let light through. This is done as a walk-in procedure in the OPD setting.
Other OPD equipment
Apart from the diagnostic equipment already mentioned in the earlier section, a typical OPD set-up in an eye hospital would also include an ophthalmic chair and lensometer (a lensometer enables us to find the power of, i.e the sphere, cylinder, axis, and prism present in each lens, if we do not know the power of the existing spectacles).
OT & Recovery medical equipment for eye hospital
A typical surgical set-up apart from the main equipment like Phaco machine and operating microscope include an OT Table, anesthesia machine, suction apparatus, multi-para patient monitor, ECG machine, sterilization equipment (such as table-top and/or vertical autoclave and bins), sealing machine, scrub sinks, fogging machine, operating instruments, OT Light/ Spot light, instrument trolleys/stands, patient trolley and a few recovery beds. The OT needs to be a highly sterile environment with low cost and easy to maintain epoxy floors and walls and anti-bacterial paint for the roof.
Download a list of equipment required for Eye Hospital with cost estimates @ just Rs 500.
Download Eye Hospital Equipment List for just Rs 500
Or Call us on +917019759765
———————————————————————————————————————————
Contact PrimedeQ on +917019759765 or +918971223957 or write to us at [email protected] to buy or sell ophthal equipment.
