WHAT IS A VENTILATOR?
Mechanical ventilation is a life support treatment. A mechanical ventilator is a machine that helps people breathe when they are not able to breathe enough on their own. The mechanical ventilator is also called a ventilator, respirator, or breathing machine. Most patients who need support from a ventilator because of severe illness are cared for in a hospital’s intensive care unit (ICU). People who need a ventilator for a longer time may be in a regular unit of a hospital, a rehabilitation facility, or cared for at home.
IMPORTANT PARAMETERS
The most important parameters to program in mechanical ventilation are the
• Ventilation mode, (volume, pressure or dual),
• Modality (controlled, assisted, support ventilation), and
• Respiratory parameters.
The main respiratory parameters are
• tidal volume and minute volume in volume modalities,
• peak pressure (in pressure modalities),
• respiratory frequency,
• positive end-expiratory pressure (PEEP),
• inspiratory time,
• inspiratory flow,
• inspiratory-to-expiratory ratio,
• time of pause,
• trigger sensitivity,
• support pressure, and
• expiratory trigger sensitivity.
Moreover, to detect problems in the ventilator and changes in the patient, alarms for tidal and minute volume, peak pressure, respiratory frequency, FiO2, and apnea must be programmed.

BRIEF ON MODES OF VENTILATION
• A mode of ventilation is the way the machine ventilates the patients and how much the patient will participate in his own ventilator pattern.
• Each mode is different in determining how much work of breathing the patient has to do.
VOLUME MODES
• Assist-control (A/C) mode
• Synchronized intermittent mandatory ventilation (SIMV) mode.
Assist Control Mode -A/C
• The ventilator provides the patient with a pre-set tidal volume at a pre-set rate and the patient may initiate a breath on his own, but the ventilator assists by delivering a specified tidal volume to the patient.
• This mode of ventilation is often used fully to support a patient, such as
• When the patient is first intubated
• When the patient is too weak to perform the work of breathing
Advantages:
• Ensures ventilator support during every breath
• Each breath has the same tidal volume
Disadvantages:
• Hyperventilation
• Air trapping
• Work of breathing may be increased if sensitivity or flow rate is too low.
Synchronized Intermittent Mandatory Ventilation- SIMV
• The ventilator provides the patient with a pre-set number of breaths/minute at a specified tidal volume and fio2.
• In between the ventilator-delivered breaths, the patient is able to breathe spontaneously. The ventilator does not assist the spontaneous breaths i.e. the patient determines the respiratory rate and tidal volume.
• This mode of ventilation is used to wean the patient from the mechanical ventilator.
• To wean the patient, the mandatory breaths were gradually decreased, thereby allowing the patient to assume more and more of the work of breathing.
• Often used as an initial mode of ventilation and for weaning
Advantages:
• Allows spontaneous breaths (tidal volume determined by the patient) between ventilator breaths;
• Weaning is accomplished by gradually lowering the set rate and allowing the patient to assume more work
Disadvantages:
• Patient-ventilator asynchrony possible
Pressure Modes
• Pressure-controlled ventilation (PCV) mode,
• Pressure-support ventilation (PSV) mode,
• Continuous positive airway pressure (CPAP)/PEEP mode,
• Noninvasive bi-level positive airway pressure ventilation (BiPAP) mode.
Control Mode CM
Continuous Mandatory Ventilation (CMV)
• Ventilation is completely provided by the mechanical ventilator with a preset tidal volume, respiratory rate and oxygen concentration prescribed by the physician.
• Ventilator totally controls the patient’s ventilation i.e. the ventilator initiates and controls both the volume delivered and the frequency of breath.
• This mode of ventilation is often used when,
• The patient does not breathe spontaneously.
• The patient can not initiate breathe
1- Pressure-Controlled Ventilation Mode ( PCV)
• The PCV mode is used to control plateau pressures in conditions such as ARDS where compliance is decreased and the risk of barotraumas is high.
• It is used when the patient has persistent oxygenation problems despite high FIO2 and high levels of PEEP.
• The inspiratory pressure level, respiratory rate, and inspiratory-expiratory (I: E) the ratio must be selected.
• Tidal volume varies with compliance and airway resistance and must be closely monitored.
Disadvantages:
• Patient-ventilator asynchrony possible, necessitating sedation/paralysis
2- Pressure Support Ventilation ( PSV)
• The patient breathes spontaneously while the ventilator applies a pre-determined amount of positive pressure to the airways upon inspiration.
• Pressure support ventilation augments the patient’s spontaneous breaths with positive pressure boost during inspiration i.e. assisting each spontaneous inspiration.
• Helps to overcome airway resistance and reducing the work of breathing.
• Patient must initiate all pressure support breaths.
• Pressure support ventilation may be combined with other modes such as SIMV or used alone for a spontaneously breathing patient.
• Indicated for patients with small spontaneous tidal volume and difficult to wean patients.
• It is a mode used primarily for weaning from mechanical ventilation.
• In general, if compliance decreases or resistance increases, tidal volume decreases and respiratory rate increases.
• PSV mode should be used with caution in patients with
• Bronchospasm
• Other reactive airway conditions.
• Used as a weaning mode, and in some cases of dyssynchrony
3- Continuous Positive Airway Pressure CPAP
• It is a variation of PEEP
• Positive pressure applied at the end of expiration during spontaneous breaths i.e. for patients breathing spontaneously.
• No mandatory breaths (ventilator-initiated are delivered in this mode)
• All ventilation is spontaneously initiated by the patient.
• PEEP & CPAP are used in patients with hypoxemia refractory to oxygen therapy. They improve oxygenation by opening collapsed alveoli & preventing them from collapsing at the end of expiration.
• CPAP allows the nurse to observe the ability of the patient to breathe spontaneously while still on the ventilator.
• CPAP is supplied during spontaneous breathing. PEEP is the term used to describe positive end-expiratory pressure with positive-pressure (machine) breaths. CPAP assists spontaneously breathing patients to improve their oxygenation by elevating the end-expiratory pressure in the lungs throughout the respiratory cycle.
• CPAP can be used for intubated and non intubated patients.
Advantages:
• Used in intubated or non intubated patients
Disadvantages:
• On some systems, no alarm if the respiratory rate falls
• Monitor for increased work of breathing.
4- Noninvasive Bilateral Positive Airway Pressure Ventilation (BiPAP)
• BiPAP is a noninvasive form of mechanical ventilation provided by means of a nasal mask or nasal prongs or a full-face mask.
• It is used in the treatment of:-
• Patients with chronic respiratory insufficiency to manage acute or chronic respiratory failure without intubations and conventional mechanical ventilation.
• Used as a bridge to weaning patients from mechanical ventilation,
• As an alternative to conventional mechanical ventilation in patients who are ventilated in their homes.
Advantages:
• Decreased cost when patients can be cared for at home;
• No need for an artificial airway
Disadvantages:
• Patient discomfort or claustrophobia
• Gastric distension
• Air leaks from the mouth

BRIEF ON PARAMETERS OF VENTILATION
Volume Modalities
• Tidal Volume
It is the volume of air delivered to a patient during a ventilator breath i.e the amount of air inspired and expired with each breath.
(Usual volume selected is between 5 to 15 ml/ kg body weight)
In the volume ventilator, Tidal volumes of 10 to 15 ml/kg of body weight were traditionally used.
The Tidal volume (ml/kg body wt) Normal range 5-7
• Minute Volume
It is the volume of expired air in one minute.
– Respiratory rate time’s tidal volume equals minute ventilation
– VE = (VT x F)
– Minute volume determines alveolar ventilation.
– Increasing the minute volume decreases the PaCO2. Conversely, decreasing the minute volume increases the PaCO2.
Pressure Modalities
• Peak Pressure
In adults if the peak airway pressure is persistently above 45 cmH2O, the risk of barotrauma is increased and efforts should be made to try to reduce the peak airway pressure.
In infants and children it is unclear what level of peak pressure may cause damage. In general, keeping peak pressures below 30 is desirable.
The fraction of inspired oxygen (FIO2)
The percent of oxygen concentration that the patient is receiving from the ventilator.
Normal r ate is between 21% & 100%
ate is between 21% & 100%
Respiratory Frequency
• Respiratory rate (breaths/min).
A person’s respiratory frequency is the number of breaths taken per minute.
The normal respiration rate for an adult at rest is 12 to 20 breaths per minute. A respiration rate under 12 or over 25 breaths per minute while resting is considered abnormal.
Positive End-Expiratory Pressure
Positive pressure applied at the end of expiration during ventilator breaths.
– The PEEP control adjusts the pressure that is maintained in the lungs at the end of expiration.
– PEEP can be visualized on the respiratory pressure gauge or display.

Instead of returning to zero (atmospheric pressure) at the end of expiration, the pressure value drops to the PEEP level.
Inspiratory Time
The inspiratory time is the time taken for inhalation. The inspiratory time is the amount of time it takes to deliver the tidal volume of air to the lung.
Inspiratory-To-Expiratory Ratio
Inspiration is normally an active process. Expiration is passive, and usually longer than the time required for exhalation, resulting in a no-flow period.
When breathing spontaneously, the work of breathing is minimised by keeping inspiratory times short and tidal volumes low just enough to get rid of the produced CO2. It is likely that the optimal I:E ratio under anesthesia is 1:1, not 1:2. A good starting point is a respiratory rate about 12 at an I:E ratio of 1:1. Normal I:E ratio at rest and while asleep is 1:2 or less.
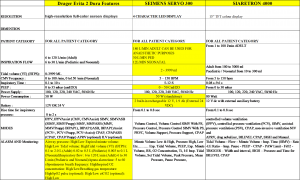
COMPARISON AND CHOICE OF THE BEST VENTILATOR
If you were to choose among ventilators of the same generation, they are almost similar in technical terms. Hence the choice of ventilator nowadays has a lot to do with accuracy of results and convenience in usage, not to mention cost-effectiveness. Ergonomics and user comfort plays a big part in ensuring there is minimal user error. The following is a simple comparison chart for reference: